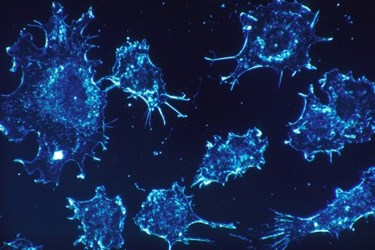
Tumor-Blasting Endoscope Seeks And Destroys Cancer Cells
By Chuck Seegert, Ph.D.
Often used to examine internal organs for tumors or other diseases, endoscopes may soon be used to treat cancer. Using new imaging methods and focused light beams, these devices may decrease side effects by delivering localized chemotherapy to tumors, thus improving treatment efficiency.
Endoscopes have long been used in a myriad of biomedical applications. The long tube-like instruments include lights and cameras and have been used for procedures like minimally invasive surgery and visualizing the interior of the gastrointestinal tract. Their long, thin geometry allows them to access many hard-to-reach areas while minimally disrupting delicate tissues in close proximity to where they are being deployed. Unfortunately, however, their capabilities are limited when it comes to imaging tumors.
Because tissues scatter or absorb light, images of the tumor environment may be blurred or have contrast levels that are too low for doctors to effectively visualize tumors. A new endoscope from University at Buffalo (UB) researchers, however, overcomes these shortcomings through spatial frequency domain imaging, according to a recent press release from UB. By projecting many different frequencies of light on the tumor, a high-contrast map can be developed that highlights the tumor and its surrounding environment.
Once identified and clearly visualized, “zapping” the tumor is the next step facilitated by the new endoscope, according to the press release. Local delivery of chemotherapy is enabled through nanoballoons, or tiny liposomes that encapsulate a drug. Though nanoballoons are administered systemically, they are only induced to release their payload when they are exposed to light from the endoscope. To carefully target the tumor, a digital mask tightly controls the shape of the light beam from the endoscope down to the micron scale. This minimizes exposure of healthy tissue to the toxic chemotherapeutic agents delivered by the nanoballoons.
“The mask is sort of like the Bat signal from Batman movies. It alters the shape of the light,” said Ulas Sunar, Ph.D., a research assistant professor at UB’s Department of Biomedical Engineering and the lead researcher of the new technology, in the press release. “At the same time, we’ll be able to control the strength of the light. The combination will allow us to manipulate the beam to target cancer cells with unprecedented accuracy.”
Using light-activated treatment systems promises to provide many advantages when enhancing the efficacy of chemotherapy. Systemically administering anticancer drugs followed by tissue-penetrating light activation allows the spatial and temporal control of drug release.
